If there is a silver lining that can be found in the great social distancing divide of 2020-2021, it is the advent of a more streamlined way to access health care services virtually anytime and from anywhere. Telehealth, Telemedicine or Virtual Visits, which are rooted in the Puget Sound, have flowered here.
Armed with the versatile, wireless devices in our pockets, we have bridged the gap carved out by the novel coronavirus. The realization: Staying in touch with our health care providers need not occur solely in vivo, through direct physical contact with another human organism. A health care examination, diagnosis, and treatment plan, can be made in vitro, through the gleaming, reflective glass of a smartphone, tablet, laptop or desktop PC.
The scourge of an invisible agent like COVID-19, or any contagious illness for that matter, make the notion of being confined to a waiting room, surrounded by other patients, something worse than counter-intuitive. It is counterfactual to contagious disease prevention in the first place. Telehealth is a reality check.
If necessity is the mother of invention, then innovation is necessity’s father.
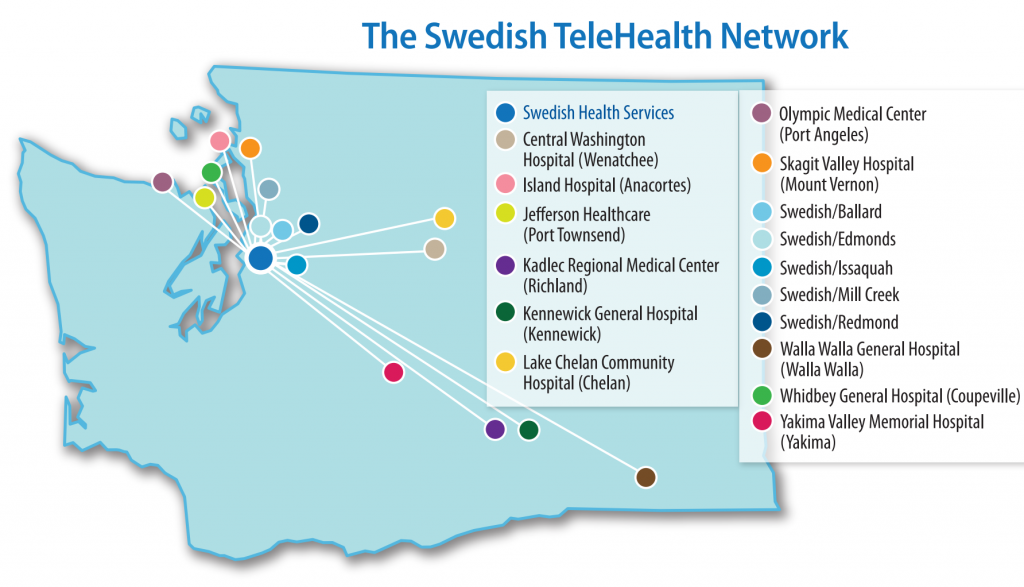
In the Pacific Northwest, Swedish Health Services, aka Swedish, has played a pioneering role in the science of telemedicine as one of our nation’s premier leaders in telehealth.

In 2004, Swedish launched TeleICU to become the first hospital in Washington – and one of a handful of hospitals nationwide – to harness technology in order to improve access to specialized care. In October 2007, Swedish launched its second telehealth program – Acute Telestroke – to use technology as a means of making available Swedish Neuroscience Institute stroke expertise to communities throughout Washington and the Pacific Northwest.
Since those early days, Swedish has added more than a dozen, specialized telehealth programs, and its network of hospitals, emergency departments and medical practices has continued to grow.
By contrast, the other virtual health care programs presented in our overview have sprung to life, in earnest, in the current Covid timeframe, starting in the spring of 2020 — emerging from the chrysalis of Internet-based, broadband communication and the ubiquity of mobile smartphone and tablet technology.
“Without overstating the case,” wrote one medical researcher, “telemedicine can sometimes deliver care that is superior to face-to-face encounters. A blood pressure reading at home may be more representative than one taken after a patient has slogged through traffic, struggled to find a parking spot, dashed into the office, and faced a battery of white coats. Veterans who suffer from PTSD may be reluctant to visit psychiatrists’ offices, but more willing to chat from home via video link.”
Timely access to telehealth applications can indeed be life-saving. In one instance, with the help of an iPad, an emergency doctor was able to listen to a patient’s breathing, observe her movements, and view a bedsore that was not healing. He quickly determined she might be in the early stages of septic shock. The patient was rushed to the hospital where she was diagnosed with a life-threatening infection.
In another example, a vacationer on a cruise ship was suffering what appeared to be an acute heart attack, or was it angina, or for that matter indigestion? Through the use of a telehealth portal, access to a cardiologist meant a timely determination on how to triage the patient.
TeleMedicine Meets TeleDemand
Conceivably, telemedicine can also smooth the growing health care demand in America and throughout the world. If a particular region is dealing with a flu epidemic, for instance, local doctors’ offices may be jammed. In such cases, remote teledoctors can relieve some of the demand and reduce the number of extra doctors, nurses, and buildings required for peak-demand periods.
Access to telehealth services can also help close the gap in the demand of physicians and the average wait time for a family practice visit. At the federal level, the Coronavirus Aid, Relief, and Economic Security Act, or CARES Act, was signed into law on March 27, 2020. Of the $27B allocated to the Public Health and Social Services Emergency Fund, $180M is to be used for telehealth and rural health activities.

In another measure designed to ease some online reporting restrictions, The Office for Civil Rights (OCR) at the Department of Health and Human Services (HHS) has announced that enforcement of HIPAA penalties around telehealth, patient communication, and remote communication technologies will be suspended during the Covid-19 National Emergency.
The telehealth programs outlined below are “non-public facing” remote communication products that allow only the intended parties to participate in the communication. They include platforms such as Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Whatsapp video chat, Zoom, or Skype. Such products may also include commonly used texting applications such as Signal, Jabber, Facebook Messenger, Google Hangouts, Whatsapp, or iMessage.

Typically, these platforms employ end-to-end encryption which allows only an individual and the person with whom the individual is communicating to see what is transmitted. The platforms also support individual user accounts, logins, and passcodes to help limit access and verify participants. In addition, participants are able to assert some degree of control over particular capabilities, such as choosing to record or not record the communication or to mute or turn off the video or audio signal at any point.
In contrast, public-facing products such as TikTok, Facebook Live, Twitch, or a public chat room are not acceptable forms of remote communication for telehealth because they are designed to be open to the public or allow wide or indiscriminate access to the communication. For example, a provider that uses Facebook Live to stream a presentation made available to all its patients about the risks of COVID-19 would not be considered a reasonably private provision of telehealth services.
Health Screening: Making the Video Connection
Dr. Nicholas Moy of Virginia Mason Internal Medicine sees video visits making a vital, human connection.
“In the setting of stay-at-home orders, being able to see our patients and still deliver care for them in the safety of their homes, helps to break through some of the isolation we are all feeling. And with universal masking, home quarantines and physical distancing, one of the most meaningful aspects for me has been the simple gift to see my patients smile the minute the video connection is live.”

“Virtual care has enabled us to continue providing our patients routine medical care and reassure them they are not forgotten during the COVID-19 crisis,” echoed Dr. Christine Palermo, Medical Director for Business Services atVirginia Mason Medical Center. “We can meet their needs wherever they are and keep them safe. Virtual care is a positive, empowering experience for my patients and for me as their doctor.”

| Provider | Virginia Mason |
| Started | March, 2020 |
| Virtual Access Name | Virginia Mason Virtual Care, Virginia Mason Virtual Clinic, and the Virtual Mason App |
| For What | Virtual Care visits are available for primary care, specialty care, chronic condition management, behavioral health, medication management, and urgent care for minor illnesses and injuries. |
| Who’s Eligible | A Primary Care Provider (PCP) referral for new patients is required. |
| Features | 24/7 access, After-visit summaries, lab test results, medical record access, health profile, online scheduling, secure doctor messaging, prescription refill requests, Benefits usage status, Choose a Doctor. Child’s records, bill payment and claims submittal |
| Technical | Desktop computer or iOS smartphone/tablet (5G or late) and the Virtual Mason App, not the VAMason App, (Android coming soon). An internet connection, and an email address to receive the link to the appointment. |
| Cost/Billing: | Virginia Mason Virtual Care visits are typically billed as an office visit, and are covered by most health insurance plans. |
| Related Services: | A standalone, on-demand, virtual clinic visit with a professional who can diagnose, treat and even prescribe medication. No appt. necessary. $59. Call (844) 733-3627. |
| Landing Page/More Info | https://www.virginiamason.org/telehealth-for-patients |
| COVID-19 Support | A COVID-19 Patient Assessment tool can be found at https://www.virginiamason.org/coronavirus |
| Provider | Seattle Children’s |
| Started | April, 2018 |
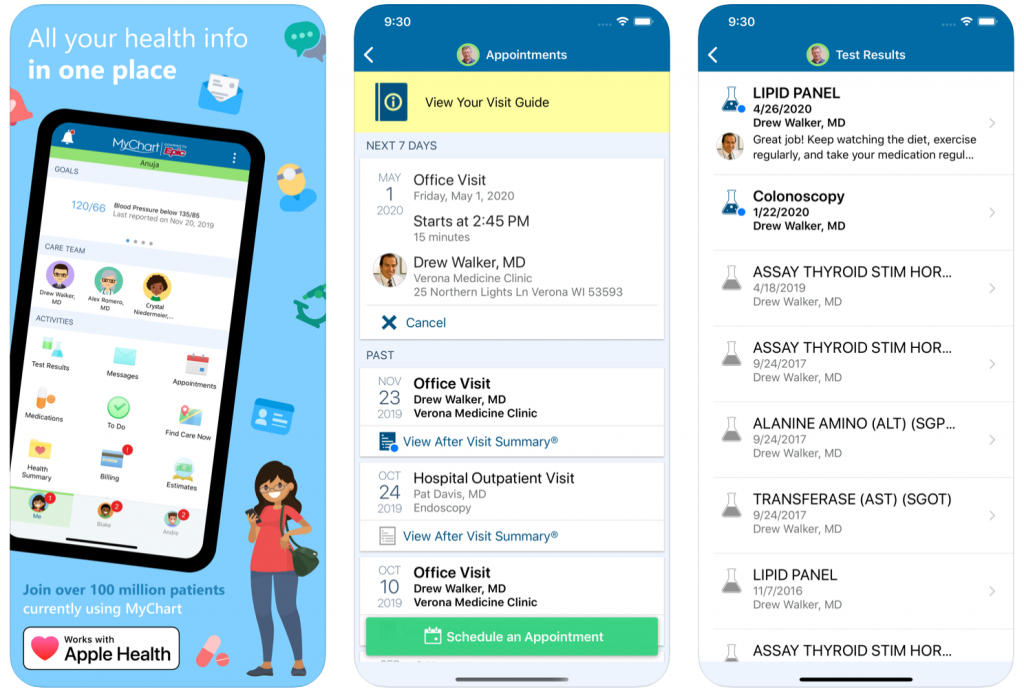
| Virtual Access Name | MySeattleChildrens, Home Telemedicine, Zoom App, MyChart Mobile App, Pharmacy Portal |
| For What | Video visits are available for any pediatric health condition that can be treated remotely. |
| Who’s Eligible | A Primary Care Provider referral for new patients is required. |
| Features | With MySeattleChildrens you can send a message to your Seattle Children’s clinic provider, check a lab and radiology result, view a medication list, clinic visit summaries and discharge instruction and view upcoming appointments. With MyChart, you have instant access 24/7 to: After-visit summaries, lab test results, Medical Record access, Health profile, Online scheduling, Secure doctor messaging, 24/7 Care Chat, Prescription refill requests. Benefits usage status. Choose a Doctor. Access child’s records. Bill payment and claims submittal |
| Technical | Download the Zoom Application to your computer, smartphone or other device that supports videos and an internet connection, as well as an email address to receive the link to the appointment. |
| Cost/Billing: | Same as in-person visit, and as a result of COVID-19 most insurance companies cover the charges in the same manner. Video visits may also be less expensive based on individual patient coverage and the absence of transportation costs. |
| Landing Page/More Info | https://www.seattlechildrens.org/clinics/telemedicine/ |

| Provider | The Polyclinic |
| Started | March, 2020 |
| Virtual Access Name | “VSee Video Visits,” MyChart Online and Mobile App |
| For What | Any health condition that doesn’t require an in-person visit. |
| Who’s Eligible | You must be a Polyclinic patient or have been granted proxy access to a Polyclinic patient’s account. A Primary Care Provider referral for new patients is required as is a Social Security number. Before their appointment, patients visit polyclinic.com/VideoVisit to access the virtual waiting room for their appointment. |
| Features | The Polyclinic uses the MyChart App for post-visit reports and doctor-patient communication. View your health summary. Get a quick snapshot of your health history, immunization record, medications, allergies, and recommended preventive services. You may also download your medical record and share your MyChart information with a healthcare professional at another organization should the need arise. Communicate with your care team. Send electronic messages and photos to your healthcare team. You can expect a reply within 48 hours. Request prescription refills. If you are out of refills at your pharmacy, you can request a renewal for a currently prescribed medication. Simply log into your MyChart account, select the medication, choose the pharmacy, and click submit. Access test results. Your lab and imaging test results will be automatically released to you online for convenient viewing and access. Schedule and view appointments. Schedule new appointments and view visit summaries from past appointments. |
| Technical | A computer, smartphone or other device that supports video, an Internet connection, and an email address to receive the link to the appointment. |
| Cost/Billing: | Video visits are billed the same as in-person office visits. |
| Landing Page/More Info | https://polyclinic.com/VideoVisitInformation https://polyclinic.com/sites/default/files/POLY-Video%20Visits%20Guide%202020%20r13.pdf |
| COVID-19 Services | Polyclinic patients can schedule a video visit to address COVID-19 concerns if one of the following symptoms is present: upper respiratory illness, cough or fever. |

| Provider | UW Medicine, Harborview Medical Center, Valley Medical Center |
| Started | March, 2020 |
| Virtual Access Name | Telehealth through UW eCare Virtual Clinic |
| For What | A video-based appointment with a UW Medicine primary care provider during regular office hours is available for annual wellness evaluations, management of chronic conditions, follow-up care and more. |
| Who’s Eligible | Patients must sign up for UW Medicine’s eCare program. To make an appointment you will need to create an account with UW Medicine’s eCare system. The process begins with obtaining an Activation Code that can be obtained here. The activation code will arrive by email and may take up to a week for processing. After scheduling your appointment by phone or eCare, you will be sent a link with information about your appointment. When it is time for your appointment to begin, you’ll click on this link to be connected with a provider. Once you have your eCare account code, you can log in here. |
| Features | Message your doctor. Securely message your doctor. Access your test results. View your results and doctor’s comments. Request prescription renewals. Send prescription renewal requests. Manage your appointments. Schedule, cancel and view details of your appointments. |
| Technical | UW Medicine uses the HIPAA-compliant Zoom video conferencing app for telehealth video conferencing. Prior to your first visit, if you want to use a tablet or smartphone, you must download the Zoom Cloud app from the Apple App Store or on Google Play. On a computer you will be asked to run Zoom once logging into the Website. You’ll be asked to enter the meeting ID which will be sent to you via email when you schedule the appointment. For the UW Medicine Virtual Clinic, you need to download the UW Virtual Clinic App from the Apple Store or the Google Play store. Download the Zoom application to your computer, smartphone or other device that supports video, an Internet connection, and email are necessary. |
| Cost/Billing: | Billing varies with insurance and financial aid may be available. |
| Related Services: | A standalone, on-demand, virtual clinic visit with a professional who can diagnose, treat and even prescribe medication. No appt. necessary. $59. Call (844) 733-3627. |
| Landing Page/More Info | https://polyclinic.com/VideoVisitInformation https://polyclinic.com/sites/default/files/POLY-Video%20Visits%20Guide%202020%20r13.pdf |
| COVID-19 Services | A UW Medicine COVID-19 Virtual Assistant can assist you with a brief walkthrough of symptom and age screening information and recommend whether you should schedule a COVID-19 gets and a telehealth appointment through UW Medicine. |

| Provider | KP Washington (formerly Group Health) |
| Started | April, 2018 |
| Virtual Access Name | KP “E-visits,” Kaiser Permanente Washington App, “My KP Meds Reminder App,” Virtual Clinic |
| For What | For common medical issues that don’t need a physical exam, such as a sore throat or allergies, go online and get a diagnosis and a treatment plan, usually within 2 hours. |
| Who’s Eligible | Employee-Sponsored Group Plans,Individual & Family Plans, SMB Plans, School Employee and Public Employee and Medicare Plans available. Members may be eligible for access by video visit email or telephone. No cost for most members. Members on a qualified HSA plan may be subject to deductibles. |
| Features | Care Chat is an online messaging feature that lets you get real-time medical care from a Kaiser Permanente care provider. Get Care — Find a doctor, schedule an appointment, contact a consulting nurse, chat with a clinician, or find Urgent Care and CareClinic locations. Medications — Refill or transfer most prescriptions, see a list of all your medications, view pharmacy wait times, or contact a Pharmacy representative. My Health — Review your health history, securely message your doctor’s office, review visit summaries, share your health record, and check most lab test results. My Plan — Pay your bill, quickly access your Kaiser Permanente Digital ID card, view Explanation of Benefits, Benefits Usage and Coverage Documents. See the Kaiser Permanente facilities nearest you, and check the wait times. |
| Technical | Computer, smartphone or other device that supports videos, an internet connection, and email. |
| Cost/Billing: | Office visits and co-pays vary by type of plan. https://thrive.kaiserpermanente.org/hello-washington/ |
| Related Services: | A standalone, on-demand, virtual clinic visit with a professional who can diagnose, treat and even prescribe medication. No appt. necessary. $59. Call (844) 733-3627. |
| Landing Page/More Info | https://my.kp.org/refreshed/my-health-manager/” |
| COVID-19 Services | On March 16, Kaiser Permanente Washington Health Research Institute (KPWHRI) gave the first-ever injection of an investigational vaccine for the 2019 novel coronavirus, SARS-CoV-2, to 4 volunteers participating in a Phase 1 federally sponsored clinical trial. The latest information can be found on the site. |


| Provider | Overlake Medical Center & Clinics |
| Started | March, 2020 |
| Virtual Access Name | Overlake Virtual Visits, MyChart App |
| For What | Virtual Visits can be used for a variety of appointments including behavioral health visits for established patients, pre- and post-operative visits, appointments for chronic illnesses like diabetes, and visits for minor conditions such as sore throats or urinary tract infections. You can also see your primary care provider virtually if you need refills on most medications. Those with Medicare/Medicare Advantage can receive Annual Wellness Visits virtually. |
| Who’s Eligible | Patients are asked to call their clinic to sign up for a virtual visit. The patient will receive a MyChart or email message with a link to connect to their provider at the scheduled visit time. If a patient needs help after hours or has concerns about symptoms of COVID-19, the patient is asked to call their provider’s clinic to reach the on-call provider, or visit one of our Urgent Care Clinics. |
| Features | After-visit summaries, lab test results, medical record access, health profile, online scheduling, secure doctor messaging, 24/7 Care Chat, Prescription refill requests, Benefits usage status, Choose a Doctor. Child’s records, Bill payment and claims submittal. |
| Technical | Computer, smartphone or other device that supports video, an internet connection, and email. |
| Cost/Billing: | Virtual visit serves as an in person visit and will be billed the same way. |
| Landing Page/More Info | https://www.overlakehospital.org/overlake-clinics/virtual-visits |
| COVID-19 Services | Use the COVID-19 Assessment Tool to answer questions or get an early screen for diagnosis. |
| Provider | Swedish |
| Started | 2004, Swedish TeleICU; 2007, Swedish Acute Telestroke |
| Virtual Access Name | Swedish Telehealth Services and/or Swedish Express Care Virtual, MyChart from Epic |
| For What | Swedish TeleHealth programs now provide over 30 different programs within the TeleHealth department including over 30 specialty disciplines, from stroke and neuroscience to TeleSleep, TeleEEG, TeleSpine, and TeleGastroenterology. |
| Who’s Eligible | Patients are asked to call their clinic to sign up for a virtual visit. The patient will receive a MyChart or email message with a link to connect to their provider at the scheduled visit time. If a patient needs help after hours or has concerns about symptoms of COVID-19, the patient is asked to call their provider’s clinic to reach the on-call provider, or visit one of our Urgent Care Clinics. |
| Features | After-visit summaries, lab test results, medical record access, health profile, online scheduling, secure doctor messaging, prescription refill requests, choose a doctor. Bill payment and claims submittal |
| Technical | Fo iOS Mobile Devices. the Swedish Heath Connect App. For Desktop: Adobe Flash Plug-In v10.1 or greater installed. Swedish has a dedicated, secure portal for patient visits through Zoom. Enhanced security measures include encryption, meeting IDs and visit “verification” to ensure your Telehealth visit is private and secure. Technical Support at 855-360-5472. |
| Cost/Billing: | Virtual visit serves as an in person visit and will be billed the same way. |
| Landing Page/More Info | https://www.swedish.org/services/telehealth-visits |
| Related Services | Express Care Virtual is designed for on-demand care so no appointment is necessary. After you register and log in, the providers who are available for an on-demand visit will appear on your screen. Under the available provider, select the green “connect” button. A virtual visit is $49 (which is reimbursable based on your insurance), payable at the time of visit via credit card. This cost does not include the cost of any medications, follow-up lab work or follow-up visits if deemed applicable. |
| COVID-19 Services | Swedish has a free COVID-19 screening tool. COVID-19 ASL videos are featured here. |
Now that you have healthcare at your fingertips, what does the future hold in store?
Experts agree that we will continue to see an evolution of smart technology built around the patient. Devices like the Apple Watch, as one example, will be linked with artificial intelligence to be able to monitor individual health around the clock. Additional sensors will provide supplemental scrutiny of the chronically ill or elderly.
“We’re going to gradually move to a world where those devices will detect something wrong with you before you even know you are sick,” reported HealthLeader magazine.
Data will feed into a system that includes the electronic medical record; that system will evaluate the input and determine what type of intervention is necessary. Within a matter of seconds, an appropriate provider will show up on the individual’s phone, tablet, computer, or television to provide guidance or care.
The global pandemic, while a godawful blight on our society and humanity, has hastened the arrival of Telehealth in providing that level of care. [24×7]